When Is Open Enrollment for Health Insurance Again in 2017
Health INSURANCE MARKETPLACES 2022 OPEN ENROLLMENT Catamenia
Final enrollment report: November 1, 2022 â€" January 31, 2017
This written report summarizes enrollment activity in the individual Marketplaces [1] during the 2022 Open Enrollment Period (2017 OEP) for all 50 states and the District of Columbia. Approximately 12.ii meg [2] consumers selected or were automatically re-enrolled [3] in Marketplace plans during the 2022 OEP. An accompanying public employ file includes detailed state-level data on plan selections as well as demographic characteristics of consumers. The methodology for this written report and detailed metric definitions are included in the public use file.
The 2022 OEP Study and the accompanying public use file include data for the 39 states that use the HealthCare.gov eligibility and enrollment platform, also as for the 12 Land-Based Marketplaces (SBMs) that use their own eligibility and enrollment platforms. [4] Demographic and program data for consumers with a program selection provided by all 50 states plus DC include: gender, age, metallic level, and whether the consumer had advance payments of the premium taxation credit (APTC) or cost sharing reductions (CSR).
For the 39 states that use the HealthCare.gov platform, additional data are available, including self-reported race/ethnicity, rural location, and household income as a percent of the federal poverty level (FPL). Also included are the proportion of returning consumers who switched plans and the average premiums among consumers with APTC. For HealthCare.gov states, additional data files with information on program selections and APTC at the county and zip code levels are also provided.Â
- Approximately 12.2 meg consumers selected or were automatically re-enrolled in a Marketplace programme in the 50 states, plus DC. Xxx-ane percent of plan selections were new to the Marketplaces.
- Nationally, 83 percentage, or nearly 10.1 meg consumers, who selected a plan had premiums reduced by advance payments of the premium taxation credit (APTC).
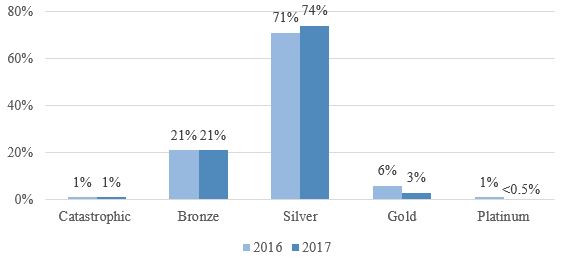
- In HealthCare.gov states, 74 percent of consumers in the 2022 OEP selected or were automatically reenrolled in silverish plans compared to 71 percent the previous yr.
Consumers Selecting Plans through the Marketplaces: 50 States, plus DC
Approximately 12.2 meg consumers selected or were automatically re-enrolled in a Marketplace program during the 2022 OEP. This includes more than ix.two one thousand thousand consumers in the 39 states using the HealthCare.gov platform and 3.0 million consumers in SBMs (come across Figure 1).
Effigy i: Programme Selections during the 2022 â€" 2022 Open Enrollment Periods [5]
Tabular array i shows the summary of enrollment by blazon for consumers who enrolled during the 2022 OEP. Thirty-one percent of consumers were new to the Market and 43 per centum of consumers actively returned to select a program on the Market place.
Table 1: Summary of 2022 OEP Program Selections by Enrollment Type
| Number | % of Full | |
| 2017 New Consumers | iii,822,114 | 31% |
| Returning Consumers Re-enrolling in 2022 Coverage | 8,393,889 | |
| Active Re-enrollees | 5,271,245 | 43% |
| Automated Re-enrollees | 2,784,013 | 23% |
| Unknown Re-enrollment type | 338,631 | 3% |
| Total 2022 Program Selections | 12,216,003 | 100% |
Table 2 summarizes selected demographic and plan characteristics for consumers during the 2022 OEP; additional data is contained in the accompanying public employ file. Thirty-half-dozen percent of all Market consumers were younger than 35 years former and 71 per centum of consumers had a silver plan. Nationally, 83 percent of consumers had their premiums reduced by APTC.
Tabular array 2: Demographic and Programme Characteristics of Consumers with 2022 OEP Plan Selections
| Age | Number[six] | % of Full[7] |
| 0 to 34 | 4,377,618 | 36% |
| 35 to 54 | four,459,781 | 37% |
| 55+ | iii,378,582 | 28% |
| Metal Level | ||
| Catastrophic | 110,821 | one% |
| Bronze | 2,802,676 | 23% |
| Silver | viii,691,150 | 71% |
| Golden | 494,969 | iv% |
| Platinum | 118,534 | 1% |
| Financial Assistance[18] | ||
| with APTC | 10,186,427 | 83% |
| with CSR[eight] | 6,826,018 | 56% |
Consumers Selecting Plans through the HealthCare.gov Platform
Additional information is available for the 9.2 million consumers in states that use HealthCare.gov. Table 3 shows selected demographic and plan characteristics among consumers who selected plans during the 2022 OEP. One-third of consumers were new to HealthCare.gov and half actively re-enrolled in coverage. 70-one percentage of consumers reported household incomes between 100% and 250% FPL. [9] Â
Table 3: Demographic and Plan Characteristics of Consumers with 2022 OEP Plan Selections on HealthCare.gov
| Consumer Type | Number | % of Full [10] |
| New consumers | 3,013,107 | 33% |
| Returning consumers who actively re-enrolled | four,560,680 | fifty% |
| Returning consumers automatically re-enrolled | one,628,018 | 18% |
| Gender | ||
| Male | iv,204,498 | 46% |
| Female person | four,997,307 | 54% |
| Location | ||
| Rural | ane,636,711 | 18% |
| Non-rural | seven,565,094 | 82% |
| Race | ||
| Asian | 600,311 | seven% |
| African-American | 660,655 | vii% |
| White | 4,446,285 | 48% |
| Multiracial and Other[11] | 145,823 | ii% |
| Unknown | three,348,731 | 36% |
| Ethnicity | ||
| Hispanic/Latino | 956,516 | 10% |
| Not Hispanic/Latino | viii,245,289 | 90% |
| Financial Aid | ||
| With APTC | 7,765,735 | 84% |
| With CSR | 5,513,078 | 60% |
| Household Income | ||
| 100% - 250% FPL | six,571,317 | 71% |
| 251%-400% | 1,539,081 | 17% |
| Other[12] | 1,091,407 | 12% |
A higher proportion of consumers selected silver plans during the 2022 OEP than in the 2022 OEP (see Figure 2). [13] Lxx-four percent of consumers in 2022 selected a silvery plan while 71 percent of consumers selected a silver plan in 2016. In both the 2022 OEP and 2022 OEP, 21 percent of consumers selected a statuary plan.
Effigy 2: Program Selections by Metallic Level amid HealthCare.gov Consumers
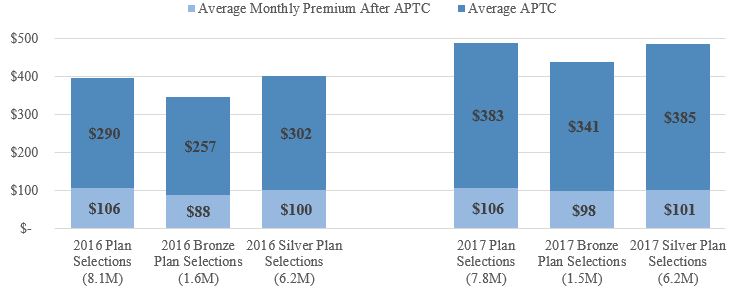
Advance payments of the premium tax credit are bachelor to reduce premiums for eligible consumers. Eighty-four per centum of consumers who selected or were automatically re-enrolled in a 2022 plan through HealthCare.gov had APTC, with an average value of $383 per person per month (see Effigy iii). [14] Among consumers with APTC, the average APTC covered well-nigh 78 percent of the gross premium, resulting in an average premium after APTC of $106 per calendar month. For those consumers who selected bronze plans and received APTC, the average premium after APTC was $88 in 2022 compared to $98 in 2017. For those consumers who selected silver plans and received APTC, the average premium after APTC was $100 in 2022 and $101 in 2017.
Figure 3: Boilerplate Monthly Premiums later APTC amid HealthCare.gov Consumers with APTC
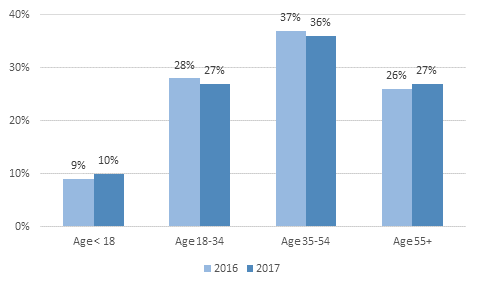
During the 2022 OEP, 10 percent of consumers were younger than 18 compared to nine percent in 2022 (see Figure iv). [15] Twenty-seven percent of consumers were betwixt 18 and 34 years old in 2022 compared to 28 percent in 2016. Twenty-seven percent of 2022 OEP consumers were 55 years or older, while 26 percent of 2022 OEP consumers were 55 years or older.
Effigy 4: Proportion of Open up Enrollment HealthCare.gov Consumers, by Age
Geographic Variation: Selected Market Metrics
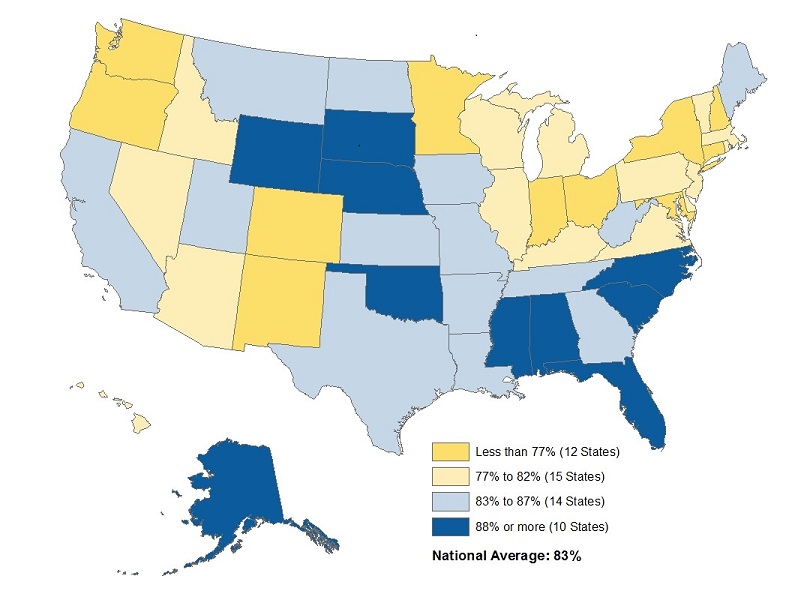
Figure five shows the proportion of Marketplace plan selections with financial assistance in the form of accelerate payments of the premium tax credit, by state. Nationally, about 83 per centum of consumers who enrolled in a plan during the 2022 OEP had premiums reduced by APTC. This ranges [16] from 59 percent of consumers in New York, to 91 percent in Nebraska.
Figure 5: Percent of 2022 OEP Marketplace Plan Selections with APTC, by State
Figure six shows the proportion of active re-enrolling consumers who switched to a new plan, by land. [17] In the 38 states using HealthCare.gov in both 2022 and 2017, about half of returning consumers switched plans. Alabama had the lowest proportion of active re-enrollees who switched plans at 31 percent, and Indiana had the highest proportion at 71 pct.
Figure 6: Percent of 2022 OEP HealthCare.gov Consumers who Switched plans, by Country
Note: Information for the 2022 program twelvemonth, through xi-1-16 through 1-31-17, tin be found at: https://www.cms.gov/Research-Statistics-Data-and-Systems/Statistics-Trends-and-Reports/Marketplace-Products/Plan_Selection_ZIP.html
[one] This written report includes Qualified Wellness Plan (QHP) plan selections made on the individual Market; an accompanying public use file besides includes data on dental plan selections and Basic Health Plan (BHP) enrollments. We do not include data for the Pocket-sized Business organisation Health Options Program (Store).
[2] In add-on to the total plan selections in this report are 764,972 individuals in New York and Minnesota signed upwards for coverage through a BHP. States accept the option of establishing BHPs to provide health coverage for depression-income residents who would might otherwise be eligible for Marketplace coverage. Without the availability of BHP, many of these consumers might instead be enrolled in a Marketplace plan.
[3] Consumers with 2022 coverage who did not make an active selection were generally automatically re-enrolled for 2017. When consumers had 2022 Market plans available to them from their 2022 issuer, they were automatically re-enrolled into the same plan as 2022 or a unlike plan from the aforementioned issuer; depending on the Marketplace, they could also be automatically re-enrolled into a suggested alternate plan from a unlike issuer.
[iv] SBM data are retrieved from the corresponding states’ data systems and take non been validated by CMS, thus metric calculations for these states may vary. The 12 SBMs are California, Colorado, Connecticut, the District of Columbia, Idaho, Maryland, Massachusetts, Minnesota, New York, Rhode Island, Vermont, and Washington.
[five] The data for the 2022 OEP was from 10/1/2013 to 4/19/2014; the 2022 OEP was from 11/15/2014 to 2/22/2015; the 2022 OEP was from 11/1/2015 to 2/1/2016 (1/31/2016 for some states); the 2022 OEP was from 11/1/2016 to i/31/2017. Plan selections past Market place model for each OEP reflects the status of the state’south Marketplace model at the fourth dimension of that OEP. Caution should be used when comparison plan selections across OEPs since some states accept transitioned platforms between years. Additionally, country expansion of Medicaid may affect enrollment figures from year to year; Louisiana expanded Medicaid in July 2016, which may have affected Market place enrollments in 2017.
[6] Some SBMs were unable to verify enrollee age and metallic level characteristics, therefore those figures exercise not sum to 12,216,003; more than information is available in the public employ file.
[7] The figures reported reverberate information every bit a percent of the full. In previous years, these figures were reported as a percent of the known (i.e. excluded “Unknown†consumers from the denominator); therefore, care should exist taken when comparing these metrics to last year. Annotation, totals may not sum to 100% due to rounding fault.
[eight] Please notation, Washington does not study its count of program selections with CSR.
[9] In 2017, for a family of four, a household income betwixt 100% and 250% of FPL by and large corresponds to an annual household income between $24,300 and $sixty,750.
[10] The figures reported reflect data every bit a percent of the total. In previous years, these figures were reported as a percent of the known (i.due east. excluded “Unknown†consumers from the denominator); therefore, care should be taken when comparing these metrics to last twelvemonth. Note, totals may not sum to 100% due to rounding fault.
[eleven] Other includes American Indian/Alaskan Native and Native Hawaiian/Pacific Islander
[12] Other includes program selections for which consumers did not provide an income, incomes beneath 100% FPL and incomes above 400% FPL. Please meet the public utilise file for more data.
[13] Kentucky switched from an SBM in 2022 to a HealthCare.gov state in 2017, thus not included in 2022 figures.
[14] Kentucky switched from an SBM in 2022 to a HealthCare.gov country in 2017, thus non included in 2022 figures.
[xv] Kentucky switched from an SBM in 2022 to a HealthCare.gov state in 2017, thus not included in 2022 figures.
[sixteen] Iv percent of consumers in the DC Marketplace have APTC. In DC, coverage in the private and minor group markets is simply bachelor through the DC Marketplace which effects the mix of consumers able to buy coverage with or without APTC.
[17] Consumers are counted equally switching plans if they picked a plan unlike from the plan they would have been machine-enrolled into had they taken no action.
[eighteen] Fiscal aid metrics were updated August 2022 to reflect changes submitted by California. Delight see the state-level PUF for more information.
Source: https://www.cms.gov/newsroom/fact-sheets/health-insurance-marketplaces-2017-open-enrollment-period-final-enrollment-report-november-1-2016


0 Response to "When Is Open Enrollment for Health Insurance Again in 2017"
Publicar un comentario